Clinical Evaluation of the Venous System of the Lower Extremity A screening examination of the venous system should be performed before performing sclerotherapy. Prior to treatment, the phlebologist must first investigate three conditions: the presence of poorly visible varicose veins proximal to or underlying the veins to be treated, deep venous or perforator valvular insufficiency, and deep venous thrombosis [5]. If there is a proximal source of superficial or deep venous reflux of blood, injection of distal telangiectasias solely will not defend against a recurrence. Subsequently, treatment of these “feeder” vessels may be necessary to ensure complete eradication of the problem. Successful sclerosis of superficial varicose veins may be rendered unsuccessful if perforating vein valvular insufficiency goes untreated.Perforating vein valvular insufficiency can lead to the development of other varicosities or telangiectasias. If the patient has deep venous valvular insufficiency, sclerotherapy of superficial varicose veins may also be inadvisable. In this setting, it is possible that the patient may encounter more severe pain when walking following sclerotherapy treatment, as the development of superficial varicose veins may have been a compensatory mechanism for an incompetent deep venous system. This is known as venous claudication [5]. Finally, because varicose veins are a risk for the development of deep venous thrombosis, a screening procedure to rule out this condition is required.
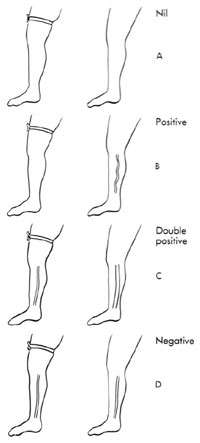
Examination of the venous system of the lower extremities can be performed without the aid of technologically advanced equipment. With the patient’s entire leg exposed, visual inspection is performed. A diagram of the visual varicosities and telangiectasias, noting bulges and fascial defects, is recorded. Importantly, fascial defects may be associated with incompetent perforator veins 50–70% of the time [4]. With the patient’s leg elevated, detection of fascial defects is performed by running the examiners finger along the course of a varicosity. Depressions within the subcutaneous tissue should be marked. Incompetence of these perforating veins can be detected by having the patient stand while the examiner holds pressure on these points. If the varicose vein fails to reappear with the patient standing, release of each finger, one at a time, distally to proximally, is performed. The release point at which the varicosity reappears is marked. This site represents the most distal incompetent perforating vein [4, 5]. A clinical sign of valvular incompetence of the saphenous venous system is demonstrated by palpating for an impulse over a segment of the greater saphenous vein when the patient coughs. The presence of an impulse with coughing implies incompetence of the valve(s) proximal to this segment (cough test) [2, 4]. The percussion/Schwartz test is performed by placing one hand over the saphenofemoral junction or the saphenopopliteal junction while the other hand is used to tap lightly on a distal portion of the long or short saphenous vein. The presence of an impulse implies valvular insufficiency in the segment between the two hands [2, 4]. Palpating over the long or short saphenous vein while tapping on a dilated tributary, or vice versa, can detect whether the tributary is in direct connection with the long or short saphenous vein. False negatives can be seen in patients with previous groin surgery, obesity, and in patients with variations in their venous anatomy. Once the dilated veins of the leg are marked, the Brodie-Trendelenburg test can be performed. With the patient in the supine position and the leg elevated 60°, emptying the varices of blood by stroking distally to proximally is performed, and a tourniquet is placed around the proximal thigh. The patient then stands up, and the leg is observed for 30 s with the tourniquet in place. The following responses can be seen:
Placing a tourniquet around the calf right below the popliteal fossae with the patient in the supine position can help to determine perforator valvular dysfunction. An indication of incompetent perforating veins occurs when the veins become more prominent and dilated as the patient ambulates [2, 4, 5]. These “hands-on” tests supply information but are not precise. These tests also do not recognize deep vein thrombosis and are not the most effective means of localizing abnormal valves. Discussion of noninvasive diagnostic techniques follows. | ||
© 2024 Skin Disease & Care | All Rights Reserved.