|
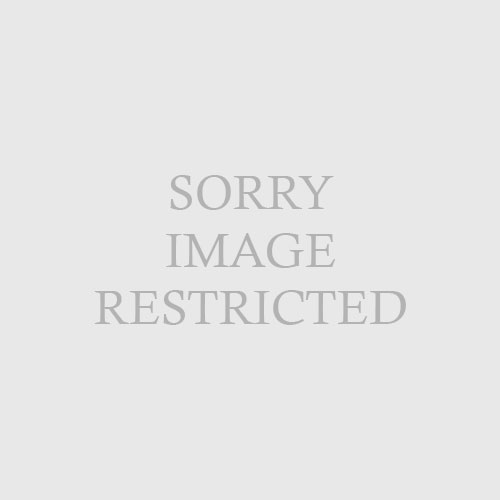
| Fig. 16.3 A, Lichen amyloidosis. Numerous pruritic, scaly papules on the anterior shin. B, Nodular amyloidosis demonstrating large waxy nodule on the nose. |
Lichen amyloidosis is the most common form of localized cutaneous amyloidosis. Lesions are pruritic, flesh-colored to brown papules, often with overlying scale (Fig. 16-3A). Papules may coalesce into verrucous plaques. The shins are the most common site of involvement. In macular amyloidosis, pruritic macular hyperpigmentation occurs most commonly in the interscapular area. The chest or extremities are less commonly involved. The lesions have a characteristic reticulate or rippled appearance. Both of these variants of primary localized cutaneous amyloidosis occur more frequently in patients from the Middle East, Asia, and Central and South America. The etiology of both lichen and macular amyloidosis is unclear but thought to be related to chronic scratching or frictional exposure. An autosomal dominant family history may be found in up to 10% of patients with lichen amyloidosis. Lichen amyloidosis is occasionally associated with multiple endocrine neoplasia type 2A.
Tanaka A, Arita K, Lai-Cheong JE, et al: New insight into mechanisms of pruritus from molecular studies on familial primary localized cutaneous amyloidosis,
Br J Dermatol 161:1217–1224, 2009.