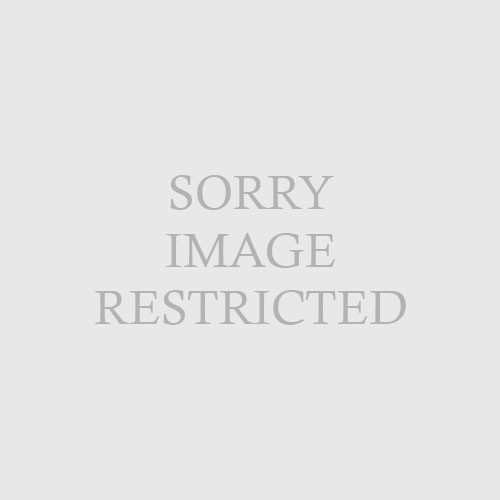
| Table 4-11 Cutaneous Tuberculosis |
| | Disease | | Clinical Findings | | Immunity/Route |
| | Scrofuloderma | | Deep nodule typically over cervical lymph node → turns fluctuant and suppurative → ulcerates
Heals with prominent scarring | | Immunity: sensitized host
(low immunity)
Route:contiguous spread (from underlying lymphadenitis) |
| | Tuberculous chancre | | Painless red-brown papule at inoculation site → nonhealing, nontender undermined ulcer with painless regional lymphadenopathy | | Immunity: non-sensitized (no prior immunity)
Route: exogenous (direct inoculation); primary infection |
| | Tuberculosis verrucosa cutis
(Warty TB) | | Small indurated hyperkeratotic papule over hand, ankle, or buttock → warty plaque with serpiginous borders
Spontaneous resolution with scarring | | Immunity: sensitized host (moderate to high immunity)
Route: exogenous
(direct inoculation at site of trauma); reinfection |
| | Lupus vulgaris | | Gelatinous reddish-brown nodules involving face or neck with brown-yellow color (“apple-jelly”) on diascopy | | Immunity: sensitized host (moderate to high immunity)
Route: hematogenous, lymphatic or contiguous |
| | Tuberculosis cutis orificialis | | Painful erythematous papule → ulcerates with undermined borders; typically in oral cavity (but can also be genitourinary) | | Immunity: sensitized host (impaired cellular immunity)
Route: autoinoculation from underlying visceral infection |
| | Miliary tuberculosis | | Tiny bluish-red papules (teeming with bacilli) which become crusted; seen mainly infants or immunosuppressed patients | | Immunity: nonsensitized
(low immunity)
Route: hematogenous dissemination |
| | Tuberculous gumma | | Firm, deep seated nodule over trunk, face, or extremities → turns soft and fluctuant → ± ulceration | | Immunity: immunosuppressed host
Route: hematogenous |
| | Papulonecrotic tuberculid | | Dusky erythematous papule → central necrosis and crust formation | | Immunity : sensitized
Route: hypersensitivity reaction to distant focus of TB (tuberculid) |
| | Lichen scrofulosorum | | Lichenoid tiny papules (tuberculids) | |
| | Erythema induratum
(Bazin disease) | | Subcutaneous inflammatory nodules with ulceration on posterior calves | | Associated with past or active TB |
| | | | | | |