The epidermis, which forms the top layer of skin, is constantly shedding millions of dead cells. It is estimated that normal skin sheds at a rate of a million cells every 40 minutes (Hinchcliffe
et al., 1999) which equates to around 18 kg over a lifetime (Marieb and Hoehn, 2007). This process of skin cell shedding is known as desquamation. As skin cells are shed, new cells are constantly pushing up from underneath to replace them. If cells develop too quickly, the skin becomes piled up and thickened (as in skin diseases such as psoriasis) and if too slowly, the skin will be thin and atrophied (as occurs in old age). The normal transit time for epidermal cells (i.e. the time they take to move from the bottom layer of the epidermis to the top layer) is around 35 days. Epidermal thickness varies over the surface of the skin and can be thought of as either ‘thick’ skin or ‘thin’ skin. Thick skin occurs on the palms and soles and has neither hair follicles nor sebaceous glands but does have sweat glands. In these areas, the epidermis is between 400 and 600 µm. Thin skin, which covers the rest of the body, has hair follicles, sebaceous glands and sweat glands and is between 75 and 150 µm thick.
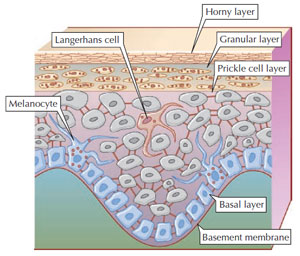
Ninety percent of epidermal cells are keratinocytes which are thought of as the building blocks of the epidermis. They start off as actively dividing cells and by the time they reach the skin surface they are anucleate bundles of keratin known as corneocytes. Keratin is synthesised within the keratinocytes from amino acids, particularly cysteine which allows for disulphide bond cross-linking which gives added strength to the skin. This is particularly predominant in hair and nails. Keratin is the same basic building block that is found in hair and nails in humans and horns, claws, hoofs and feathers in animals and birds.
|
Figure 2.2 Layers of the epidermis.
(Source: Reprinted from Graham-Brown and
Burns, 2006.) |
Other epidermal cells include melanocytes (around 8% of total number of cells) and Langerhans cells (Figure 2.2).
Basal layer Also known as the stratum basale or stratum germinativum, this is a single layer of columnar-shaped keratinocytes, some of which are stem cells undergoing constant cell division to produce new keratinocytes (Tortora and Derrickson, 2006). Each active basal cell divides every 4 days to produce daughter cells which then go on to differentiate and mature. These basal cells are ‘power-houses’ of activity containing various cellular structures which allow them to replicate effectively. Each cell has a large nucleus made up of cytoplasm containing ribosomes, which are attached to rough endoplasmic reticulum, a small Golgi complex and a few mitochondria (Table 2.1).
| | | | | | Table 2.1 Structures seen within basal cells.| | Cell structure | Activity | | | Ribosomes | Sites of protein synthesis | | | Rough endoplasmic reticulum | A network of channels that serves as intracellular transportation, supporting, packaging and transporting molecules | | | Golgi complex | Modifies, sorts, packages and transports proteins received from the endoplasmic reticulum | | | Mitochondria | Produce adenosine triphosphate (ATP), crucial for energy production |
| | | | | |
|
The basal layer also includes the melanocytes, responsible for producing melanin which gives colour to skin and hair and protection from ultraviolet (UV) radiation. The production of melanin is under genetic control and is regulated by melanocyte stimulating hormone (MSH) secreted from the anterior lobe of the pituitary gland. Clinically, it is interesting to note that MSH is very similar in structure to adrenocorticotrophic hormone (ACTH). People with increased ACTH secretion, for example in Addison’s disease, show increased pigmentation in sun-exposed sites and where they experience mild trauma (Hinchcliffe
et al., 1999) because ACTH acts as MSH.
The production of melanin occurs within organelles known as melanosomes, in the cytoplasm of the melanocytes. Within these melanosomes, the amino acid tyrosine is converted into melanin in the presence of the enzyme tyrosinase. From here it is transferred into the cytoplasm of the surrounding keratinocytes. Variations in hair pigment are caused by biochemical differences in the melanin produced in blondes, brunettes and redheads. The racial differences in skin pigment can be explained by the fact that in Caucasians, melanosomes are grouped in complexes which degenerate as the keratinocytes move towards the surface of the skin. In darker-skinned people the skin contains the same number of melanocytes, but the melanosomes are larger, remain separate and persist throughout the thickness of the epidermis (Graham-Brown and Burns, 1996). The quantity of melanin found in keratinocytes depends to a large extent on genetic make-up and the environment, that is how much UV exposure someone is subjected to.
|
Figure 2.3 Desmosome. (Source: Reprinted from
Tortora and Derrickson, 2006.) |
Finally, the epidermis contains specialised cells called Merkell cells. At the interface of the epidermis and dermis, the flattened process of a sensory neuron comes into contact with the tactile disc of the Merkell cells thus detecting certain aspects of touch and sensation. Prickle cell layer (stratum spinosum) As keratinocytes mature and differentiate, they go through the transition to the prickle cell layer where the cells become interlocked by a network of desmosomes. Desmosomes are designed specifically to hold cells together and as such are important structures which give the resilience to the skin. They consist of a plaque on either side of the plasma membrane (where a plaque is a dense layer of protein). On one side of this plaque, extending into the intracellular space, are glycoproteins known as cadherins which attach to one another. On the other side of the plaque, filaments consisting of keratin (known as tonofilaments), stretch from one side of the cell to the other where they attach to other desmosomes (Figure 2.3). This provides the cell with structural stability. The cells in this layer are so called because when they are fixed and observed under a microscope, the cells pull slightly away from each other so that the desmosomes can be seen stretching across the intracellular space giving the cells a prickle-like appearance.
The prickle cell layer of the epidermis is between 8 and 10 layers thick. Keratohyalin granules are present in the keratinocytes and they contain a substance which combines with intermediate filaments of the cytoskeleton converting them to keratin; these also contribute to the resilience of the skin. Also in this section of the skin, lipid-filled membrane coating bodies start to develop.
Langerhans cells are present in the prickle layer. These cells are highly specialised dendritic cells which are an important part of the immune system, located within the skin. They are called dendritic cells because the surface membrane is folded in a similar way to the dendrites of the nervous system. This is so that the Langerhans cells can have maximum surface area to allow interaction with other cells. As immature cells, they are highly endocytotic (i.e. their plasma membrane invaginates producing an intracellular vesicle which surrounds the ingested material). However, as the Langerhans cells differentiate they have an increased capacity to migrate to T-cell areas and to function as antigen-presenting cells (Roitt and Delves, 2001). Mature Langerhans cells are covered in molecules known as major histocompatibility complex molecules, class II. These are adept at presenting the pieces of antigen protein to T-cells, which are then destroyed (Lydyard
et al., 2000).
Granular layer (stratum granulosum) Also called the stratum granulosum, this is the part of the epidermis where there is high lysosomal activity. Lysosomes are organelles which contain enzymes that digest the cell contents causing the cell nuclei to disintegrate. At this stage the keratohyalin granules become more prominent within the cell and the lipid-filled membrane coating vesicles, which have been produced in both the granular and prickle cell layers, start to undergo exocytosis extruding the glycolipid over the keratinocyte membranes, thus helping to lubricate and waterproof the skin. These lipids include 40% ceramides, the rest being comprised of fatty acids, cholesterol and cholesterol sulphate. Langerhans cells continue to be present in the granular layer.
Horny layer (stratum corneum) The horny layer or stratum corneum is the outer layer that interfaces with the environment. It is vital that it is capable of keeping out unwanted allergens and pathogens and retaining moisture by preventing water loss by evaporation. The cells of this outer layer are fibrous, tough bundles of keratin known as corneocytes. Filaggrin, a protein, which is also seen in the cells at this point, binds with keratin to help provide an effective skin barrier. Recent research has shown that the correct functioning of filaggrin is essential for effective barrier function of the skin. Examining the genetic make-up of people who suffer from icthyosis and atopic eczema shows loss of function mutations for filaggrin which may explain why the barrier function is compromised in these individuals (Hoffjan and Stemmler, 2007).
The horny layer contains a number of substances known as natural moisturising factors (NMF). These substances which include lactic acid, pyrrolidonecarboxylic acid and urea are water loving. They attract and hold water thus helping to maintain the hydration of the horny layer. Around 15% of the stratum corneum is water, if this falls below 10% the skin will become dry. The lipids, which were produced in the prickle and granular layers, continue to be present in the horny layer. They form what is known as a lipid bilayer which helps to further fortify the barrier function of the skin.
In order to ensure the effective barrier function of the skin, all these mechanisms need to be in place.
(1)
Keratin and filaggrin: to maintain a tough barrier to keep out allergens and pathogens;
(2)
NMF: to attract and retain moisture;
(3)
Lipids: to lubricate and waterproof the skin as well as helping to trap the moisture in the stratum corneum.