Self-management and patient support The management of a chronic illness requires a number of factors to sustain effective health behaviour; this includes knowledge, skills and confidence in managing a condition long term. These areas require education and psychological support that is systematically assessed and planned. A key aspect of this support is emotional support to help individuals to cope with their long-term condition and their treatment regimens and recognition of their impact on their lifestyle. Awareness is also needed of specific issues that may affect some people, such as low self-esteem, poor motivation and a lack of social confidence. Educational and support needs reflect aspects of the person’s care that can be unmet or poorly met because their management is not necessarily systematically planned for in the same way as treatment regimens. Chronic illness management relies on a person changing their health behaviour, and specifically adaptive self-management, which in turn requires the patient to understand their condition and treatment to maintain health and improve their quality of life. Professional support is required to achieve this. An editorial in the British Medical Journal (Bodenheimer et al., 2005) has highlighted the potential key role of Nurses as leaders in chronic care, reflecting the need to combine treatment with education and support, which nurses are well placed to provide. People living with long-term conditions are high demand users of health services. There is a strong policy context urging the need to address the needs of this group, improve chronic disease management through helping to improve selfcare and the individual’s contribution to their care (Department of Health, 2004, 2005a, b).
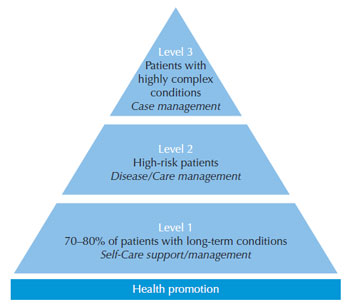
Therefore, a key challenge for the majority living with chronic conditions is to engage in effective self-management and self-care support. The Department of Health (2005a) highlighted the different levels of need for this group to which the service needed to respond (Figure 7.1). For those living with long-term conditions that are at high risk of deterioration, disease management is required to reduce risk, maintain health and reduce the need for hospital admission. A key target group are those living with complex conditions. This includes patients with multiple conditions, such as a person with psoriasis who also has active psoriatic arthropathy and other chronic conditions, e.g. diabetes. Intervention to maintain and promote the health of people living with long-term conditions requires a foundation of support to ensure that they can effectively do self-management. If people with chronic conditions are to be expected to engage in a degree of self-management, it is necessary to be clear about the expectations of the person and their carers. This provides the basis for instigating an effective plan of care and treatment and determining where support is needed to prepare the person and their family. It will also reflect where there are unmet or poorly met educational and support needs and then, where intervention is required, when there are limits to self-management or the process of self-care fails. Table 7.1 illustrates some of the complexity of helping patients to use their treatment optimally and the educational and support challenges for health professionals. These areas of health care need present nurses and other health professionals with significant therapeutic opportunities to enable or empower the person and their family to engage actively in self-management. Each area of knowledge and skill also requires a degree of confidence for the person trying to apply these.
Educational and support needs are both common and individual. As such, rigorous patient surveys can provide an indication of patterns of need that practitioners can plan to address (Krueger et al., 2001; Beresford, 2002). These needs are reflected in Table 7.1. They convey a need to understand their condition, those factors that adversely affect and improve it and their treatment. Dissatisfaction with the effectiveness of treatments is a theme running through the findings. This has been validated through recent qualitative evidence, reflecting self-management needs (Ersser and Cowdell, 2009). | |||||||||||||||||||||||||||||||||||||||||||||||
© 2025 Skin Disease & Care | All Rights Reserved.